Calcium and Thyroid Relationship
Calcium is the most abundant mineral in a human body.
This mineral has many important functions that only emphasize the need of well-balanced diet that delivers sufficient levels of calcium.
Your body needs calcium for vasodilation and vascular contraction, muscle function, nerve transmission, intracellular signaling and many other purposes.
Bearing in mind we have more calcium than any other mineral, it would be impossible not to wonder about its link with thyroid.
Let's find out more about the relationship between calcium and thyroid gland.
Calcium and thyroid hormones
Despite the fact that calcium is the most prevalent mineral in a human body its role in thyroid health is poorly understood.
While some studies have investigated this subject, the available data is still limited which only heightens the importance of more studies on the calcium-thyroid relationship.
One study tested the relationship between calcium and thyroid hormones.
For this purpose, scientists enrolled 40 adults and tested levels of calcium and thyroid hormones T3, T4, and TSH.
Results showed a weak correlation between the concentration of calcium and thyroid hormones. The increase of calcium was slightly associated with an increase of these hormones.
The calcium-sensing receptor poses as the molecular mechanism wherein parathyroid cells detect changes in the concentration of blood ionized calcium and modulate secretion of parathyroid hormone in order to maintain serum levels of the mineral in a healthy range.
It is important to mention that parathyroid refers to small glands located in the neck behind the thyroid and they control calcium.
Parathyroid hormone stimulates the bone reabsorbing releasing calcium in extracellular fluid and the increased levels of the mineral occur due to improved absorption of calcium and the rapid effect of parathyroid hormone to decrease exertion of calcium by kidneys.
This particular effect can lead to an increase in T3. In addition, renal calcium influenced by thyroid hormone was higher in hypothyroidism and lower in hyperthyroidism.
Serum levels of this important mineral decreased significantly in participants with high TSH. Evidence also shows that calcium can decrease the activity of the thyroid and its absorption may lead to insufficiency in the hormones produced by the gland[i].
Hyperthyroidism and calcium levels
Studies also demonstrate that abnormal thyroid function has the ability to alter the metabolism of this mineral.
Back in 1929, it was discovered that fecal and urinary excretion of calcium is frequently increased in hyperthyroidism and lower than normal myxedema (a life-threatening complication of hypothyroidism).
These changes in calcium levels could not be associated with changes in vitamin D deficiency or some other parameters[ii].
The modern science only confirmed findings that were made decades ago.
One study revealed that the vast majority of patients with hyperthyroidism in the West have normal or increased total calcium levels and the mean plasma concentration is notably higher than in healthy controls.
The percentage of hyperthyroid patients with hypercalcemia varies from one study to another, depending on the number of participants they had.
One research showed that increased calcium levels occurred in 23% or 19 in 77 patients, while other found 5-27% and there were also studies where more than 50% of people with hyperthyroidism had elevated levels of calcium[iii].
Hypercalcemia can cause a number of symptoms such as a headache, fatigue, excessive thirst, excessive urination, abdominal pain, constipation, nausea, vomiting, abnormal heart rhythms, muscle cramps, muscle weakness, and many others[iv].
The problem with too much calcium in the body usually resolves after achieving the euthyroid state i.e. when levels of thyroid hormones normalize.
When discussing the relationship between calcium and hyperthyroidism it is important to mention that renal excretion of the mineral is increased in hyperthyroid individuals and it positively correlates with excess cortical osteoclastic activity and thyroid hormone.
This is caused by heightened mobilization of bone mineral in hyperthyroidism and higher levels of the mineral remain elevated even when a person undergoes low-calcium diet.
What about calcium and hypothyroidism?
Even though a growing body of evidence confirms higher levels of calcium are strongly associated with hyperthyroidism, it appears that metabolism of the mineral has no meaningful effect in individuals with hypothyroidism.
For example, a study whose findings were published in the Biological Trace Element investigated the status of magnesium, calcium, and zinc in hypothyroid patients. Researchers discovered that concentration of zinc decreased while levels of magnesium increased, but calcium status remained the same[v].
In addition, a research from the Endocrine Journal also found that hypothyroidism is not associated with disturbed metabolism of calcium[vi]. The Journal of Laboratory Physicians featured a study which evaluated calcium status in hypothyroid women.
Scientists discovered that hypothyroidism was associated with some changes in ionized calcium, but not total calcium. This means that the psychologically active form of the mineral could be affected, but the overall concentration is unchanged which only confirms results of previous research on the subject.
Despite the fact that calcium is not overly affected by hypothyroidism, this is still an interesting topic due to the effect of this important mineral on hypertension and heart muscle[vii].
Evidence shows that calcium is the first messenger for the thyroid hormone’s plasma membrane-mediated action to enhance uptake of cellular sugar[viii].
Moreover, thyroid hormone also produces a temporary increase of calcium uptake by your heart. Calcium contributes to high blood pressure or hypertension through its ability to lead to the increment of sodium excretion.
Lower sodium intake reduces excretion of calcium and vice versa, which only explains why calcium plays a role in a person’s blood pressure. Why is this important? It matters because hypothyroidism is a secondary cause of high blood pressure[ix].
Calcium supplementation: be careful!
Dietary supplements are practical for getting the recommended daily amounts of different vitamins and minerals.
They help us consume the required levels of these nutrients because we don’t usually get them through diet.
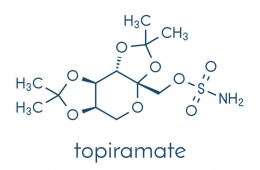
While supplementation with different minerals and vitamins proves to be beneficial for patients with some thyroid problems, that is not the case with calcium. In fact, if you have hypothyroidism and are taking levothyroxine (T4) you should probably consult your doctor before taking calcium supplements.
A study of 20 patients from the JAMA discovered that calcium reduces the absorption of T4 while increasing thyrotropin levels. Levothyroxine adsorbs to calcium in an acidic environment, thus reducing its bioavailability[x].
A study from the journal Thyroid also discovered that consumption of calcium supplements interferes with absorption of levothyroxine[xi].
Bearing in mind that calcium is necessary for a number of functions in our body, especially for strong bones, supplementation is for many people the best way to avoid complications associated with low calcium.
If you don’t get enough of this mineral through your diet and want to take a supplement, but at the same time if you’re taking levothyroxine, you should consult your doctor first. In fact, if your doctor is about to prescribe levothyroxine, feel free to mention that you are taking calcium supplements too. Your physician will explain whether it’s safe for you to continue taking them and what to do net.
The same thing you should do if you’re taking levothyroxine and you’re considering taking calcium supplement – ask your doctor. Hypothyroidism is a unique situation, every decision you make has an impact on your treatment.
Also, make sure you do not take a calcium supplement and levothyroxine together; they should be taken at least three hours apart from one another. The same goes for products that contain calcium, avoid consuming them around the same time you take levothyroxine.
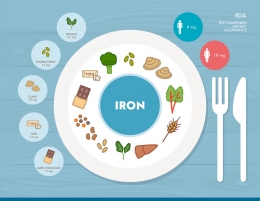
How much calcium do I need?
As mentioned above, taking recommended daily value of different nutrients (including calcium) is essential for proper functioning of your body.
Recommended daily intake of calcium according to the National Institutes of Health is[xii]:
- 0-6 months: 200 mg
- 7-12 months: 260 mg
- 1-3 years: 700 mg
- 4-8 years: 1000 mg
- 9-13 years: 1300 mg
- 14-18 years: 1300 mg
- 19-50 years: 1000 mg
- 51-70 years: 1000 mg for men and 1200 mg for women
- 71+years: 1200 mg
What if I have hypercalcemia due to hyperthyroidism?
Earlier in the post, we have mentioned that numerous studies found the link between hyperthyroidism and higher levels of calcium.
Hypercalcemia induces a wide range of symptoms and it is a threat to your health, but it is a manageable condition. The most effective way to overcome hypercalcemia is to treat the underlying condition or in this case hyperthyroidism.
You may also consult your doctor or a nutritionist about low calcium diet until thyroid hormone levels normalize, which would also establish calcium balance too. Staying hydrated throughout the day is also recommended and you should also strive to be physically active.
Sources of calcium
A well-balanced diet is an important pillar of a healthy lifestyle and you should strive to get the required amounts of calcium through your diet. We tend to associate calcium with milk only, but there are many other food sources of this mineral.
The best sources of calcium include:
- Beans – legumes are also a great source of calcium but winged beans have the highest content of 24% recommended daily intake (RDI) or 244mg calcium in one cup (cooked), while one cup of cooked white beans have 13% RDI calcium
- Canned salmon and sardines – yes, fish is also a good source of calcium. In fact, three ounces of canned salmon with bones supplies your body with 21% RDI of this mineral while a 3.75-ounce can of sardines has 35% RDI of this mineral
- Cheese – almost every cheese is an excellent source of calcium with parmesan being the richest in this mineral with 331mg or 33% RDI per ounce or 28g. Generally, soft cheeses usually have a lower amount of calcium than their counterparts. For instance, an ounce of brie delivers 52mg calcium or 5% RDI
- Seeds – poppy, chia, celery and sesame seeds are a surprisingly abundant source of calcium. For example, one tablespoon (15g) of poppy seeds delivers 126mg of calcium, which is about 13% RDI. On the other hand, one tablespoon of sesame seeds has 9% RDI calcium. Let’s not forget that seeds are an excellent plant-based source of essential Omega-3 fatty acids
- Tofu – that is prepared with calcium supplies your body with 86% of RDI
- Yogurt – one cup or 245g of plain white yogurt supplies the body with 30% RDI calcium while low-fat yogurt has 45% RDI in one cup. Greek yogurt is widely popular today but it is lower in calcium than “regular” yogurt
Conclusion
Our body consists of different vitamins and minerals. Calcium is the most plentiful mineral in your body and it takes part in many functions.
Studies show that hyperthyroidism is associated with elevated levels of calcium and may also lead to hypercalcemia. Luckily, treatment of hyperthyroidism and normalizing levels of thyroid hormones can also manage high calcium levels.
On the other hand, calcium status is usually unaffected in hypothyroid patients, but this subject requires more research due to the impact of this mineral on blood pressure. If you’re hypothyroid and want to take calcium supplements, consult your doctor first.
References
[i] Abduallah JA, Abdulkalek H, Haider S, Aamer A. Study of the relationship between calcium ion and thyroid hormones, liver enzymes in some patients with hypocalcaemia and hypercalcaemia. Journal of Contemporary Medical Sciences 2015 Summer, vol. 1 no. 3, 27-30. ISSN 2413-0516 http://www.jocms.org/index.php/jcms/article/view/30
[ii] Krane SM, Brownell GL, Stanbury JB, Corrigan H. THE EFFECT OF THYROID DISEASE ON CALCIUM METABOLISM IN MAN . Journal of Clinical Investigation. 1956;35(8):874-887. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC441658/?page=1
[iii] Dhanwal DK. Thyroid disorders and bone mineral metabolism. Indian Journal of Endocrinology and Metabolism. 2011;15(Suppl2):S107-S112. doi:10.4103/2230-8210.83339. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3169869/
[iv] Hypercalcemia: what happens if you have too much calcium? Healthline.com https://www.healthline.com/health/hypercalcemia#overview1
[v] Simsek G, Andican G, Karakoc Y, et al. Calcium, magnesium, and zinc status in experimental hypothyroidism. Biological Trace Element 1997 Feb, 60.3, 205-13 https://search.proquest.com/openview/ad4edb9e4b624065ad2a0f8d56d6c50f/1?pq-origsite=gscholar&cbl=54117
[vi] Kisakol G, Kaya A, Gonen S, Tunc R. Bone and calcium metabolism in subclinical autoimmune hyperthyroidism and hypothyroidism. Endocrine Journal 2003 Dec, vol. 50 no. 6, 657-661. Doi: 10.1507/endocrj.50.657 https://www.jstage.jst.go.jp/article/endocrj/50/6/50_6_657/_article
[vii] Al-Hakeim HK. Serum Levels of Lipids, Calcium and Magnesium in Women with Hypothyroidism and Cardiovascular Diseases. Journal of Laboratory Physicians. 2009;1(2):49-52. doi:10.4103/0974-2727.59698. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3167967/
[viii] Segal J. Calcium is the first messenger for the action of thyroid hormone at the level of the plasma membrane: first evidence for an acute effect of thyroid hormone on calcium uptake in the heart. Endocrinology 1990 May;126(5):2693-702. Doi: 10.1210/endo-126-5-2693 https://www.ncbi.nlm.nih.gov/pubmed/2328703/
[ix] Stabouli S, Papakatsika S, Kotsis V. Hypothyroidism and hypertension. Expert Review of Cardiovascular Therapy 2010 Nov;8(11):1559-65. Doi: 10.1586/erc.10.141 https://www.ncbi.nlm.nih.gov/pubmed/21090931
[x] Singh N, Singh PN, Hershman JM. Effect of calcium carbonate on the absorption of levothyroxine. JAMA 2000 Jun;283(21):2822-2825. Doi: 10.1001/jama.283.21.2822 https://jamanetwork.com/journals/jama/fullarticle/192748
[xi] Zamfirescu I, Carlson HE. Absorption of Levothyroxine When Coadministered with Various Calcium Formulations. Thyroid. 2011;21(5):483-486. doi:10.1089/thy.2010.0296. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3092723/
[xii] Calcium, National Institutes of Health https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/


























































Leave a comment