Hashimoto's and Estrogen Dominance
The balance of hormones in our body is crucial for overall health and wellbeing.
Increased or decreased levels of some hormone can induce a domino effect or chain of reactions that affect other hormones as well.
For example, estrogen-related imbalances can contribute to problems with thyroid hormones and vice versa.
Estrogen dominance is a common problem and we are going to discuss its relationship with Hashimoto’s thyroiditis in this article.
What is estrogen dominance?
Estrogen dominance is a well-known term, but most of us are not quite sure what it entails.
What does it actually mean?
Estrogen dominance is defined as a metabolic state where estrogen levels are higher than progesterone concentration in a woman’s body.
In other words, this condition occurs when there is too much estrogen in the body, but an insufficient amount or total lack of progesterone to counter fight it.
The term “estrogen dominance” was coined two decades ago, in 1996, by John R. Lee and Virginia Hopkins who described this condition in their book What Your Doctor May Not Tell You About Menopause: The Breakthrough Book on Natural Progesterone. Ever since then, estrogen dominance has become a frequently discussed topic in relation to menopause, but its effects go much deeper than that.
How does estrogen dominance happen?
Although estrogen dominance is a common problem that affects millions of women, the underlying mechanisms are still quite unclear.
Patel et al. report that while the normal aging process is supposed to lower estrogen levels the increment in inflammatory agents in everyday life are increasing the estrogen and estrogen mimic levels thus fueling a condition called estrogen dominance.
The resulting excess estrogen induces overexpression of estrogen receptors and harms tissues, paves the way to autoimmune diseases, among other things. Estrogen dominance, then, leads to other problems such as polycystic ovary syndrome (PCOS), ovary cancer, and breast cancer[i].
In order to understand how estrogen dominance develops, it's important to know how the menstrual cycle works.
Basically, estrogen is a dominant hormone for the first two weeks of the menstrual cycle until the ovulation when it is balanced by progesterone. Generally speaking, as a woman enters perimenopause estrogen can become unopposed i.e., progesterone levels are low or nonexistent so they can't oppose this dominant hormone.
That's when estrogen dominance occurs, and various symptoms show up. However, you need to bear in mind that skipping ovulation is only one potential factor that plays a role in the development of estrogen dominance.
Other factors that can make you estrogen dominant include overweight or obesity, environmental factors, and exposure to endocrine disruptors, impaired immune function, low-fiber diet, and unmanaged stress.
What are the symptoms of estrogen dominance?
When hormone levels are not in balance, our body feels it in more ways than one.
Estrogen dominance is not an exception. High levels of estrogen can manifest themselves in different ways, and symptoms range from mild to severe. Not every woman experiences the same symptoms in equal intensity.
Some of the most common signs and symptoms of estrogen dominance are:
- Irregular menstrual cycle (no periods at all or heavy periods)
- Trouble sleeping
- Swollen and tender breasts
- Memory problems
- Low sex drive
- Lethargy
- Hair loss
- Fibrocystic breast lumps
- Weight gain
- Enhanced symptoms of PMS
- Cold hands and feet
- Anxiety
- Mood swings
- Headache
- Bloating or water retention
- Slow metabolism
- Thyroid dysfunction
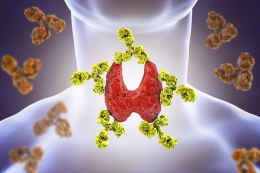
How is estrogen dominance linked with Hashimoto’s thyroiditis?
Take a look at the last symptom of estrogen dominance in the section above. As you can see, greater levels of estrogen are associated with dysfunction of the thyroid gland.
Hashimoto's thyroiditis happens to be an autoimmune condition and the most common cause of underactive thyroid i.e., hypothyroidism.
This information tells us that estrogen dominance and Hashimoto's thyroiditis could be related, but let's dig deeper to evaluate the relationship between two conditions.
Estrogen dominance can, oftentimes, be mistaken for Hashimoto’s or hypothyroidism due to the fact they share similar symptoms.
Both thyroid dysfunction and estrogen dominance can contribute to weight gain, slow metabolism, mood swings, cold feet and hands, hair loss, memory problems, fatigue, just to name a few.
For that purpose it is crucial to see your doctor, report all symptoms and changes in the body you experience and based on tests and physical exam your healthcare provider will be able to diagnose the health problem.
Hashimoto’s thyroiditis common in PCOS patients
Even though studies on the subject of estrogen dominance and Hashimoto’s thyroiditis are limited, current evidence shows there is a link between them.
For instance, in a study by Arduc et al. a positive relationship between PCOS and Hashimoto's thyroiditis was observed.
The study included 86 reproductive-age women who were diagnosed with PCOS and 60 age-BMI matched healthy controls.
Scientists tested their thyroid hormone levels, estrogen, androgens, progesterone, insulin, fasting glucose, performed pelvic, and thyroid ultrasounds. Results of the study showed that women with PCOS had higher levels of TSH, anti-TPO, testosterone, and lower levels of progesterone.
Hashimoto’s thyroiditis was more common in women with PCOS than in their healthy counterparts. Scientists concluded the study confirming that there is a higher prevalence of Hashimoto’s thyroiditis in patients with estrogen dominance. Higher estrogen and estrogen-progesterone ratio could be involved directly in elevated anti-TPO levels in women with polycystic ovary syndrome[ii].
Basically, this study is perfect evidence that Hashimoto's thyroiditis and estrogen dominance are strongly related. It connected Hashimoto's disease with PCOS, which happens due to estrogen dominance and also showed that patients had higher estrogen and lower progesterone levels.
Estrogen suppresses thyroid hormones
One potential mechanism that could explain the relationship between estrogen dominance and Hashimoto’s thyroiditis is the very nature of the estrogen – thyroid connection.
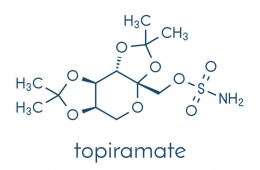
Evidence confirms that estrogen has an indirect impact on thyroid economy by elevating the levels of thyroxine-binding globulin and increasing the necessity for thyroid hormone in women with hypothyroidism[iii].
Estrogen levels could affect thyroid function and lead to thyroid disorders by impairing the functionality of thyroid receptors. These receptors allow thyroid hormones to enter cells. When their function is impaired, they are unable to do their job, thus affecting the levels of thyroid hormones in the body.
In other words, estrogen has the ability to suppress thyroid hormone and elevates the need for TSH. On the other hand, progesterone stimulates thyroid hormones. In estrogen dominant women, there is no balanced action of estrogen and progesterone necessary for optimal thyroid hormone concentration.
This leads to the dysfunction that contributes to or aggravates Hashimoto’s thyroiditis and hypothyroidism.
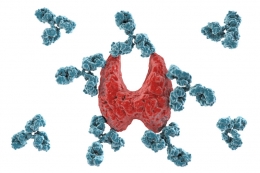
Estrogen contributes to autoimmune thyroid conditions
Estrogen dominance and Hashimoto’s thyroiditis are also connected through the connection of this hormone with the immune system.
Wang et al. reported that prolonged exposure to high levels of estrogen can boost anti-TPO antibodies and thereby contribute to autoimmune thyroid conditions[iv] such as Hashimoto’s thyroiditis. It is also worth noting that it’s challenging for the body in hypothyroid women to detoxify estrogen due to decreased function of the liver.
This can create a chain of reactions that leads to excessive estrogen levels, higher anti-TPO, autoimmunity, and a number of symptoms that can affect a woman’s quality of life. The fact that high estrogen levels lead to autoimmunity could explain why Hashimoto’s thyroiditis is more prevalent in women with this problem compared to healthy controls.
How is estrogen dominance treated?
Estrogen dominance should not be ignored. What’s more, unmanaged estrogen dominance could be the reason why Hashimoto’s thyroiditis treatment isn’t as successful as you’d want it to be.
Hormonal imbalances are not uncommon, but at the same time, they’re entirely manageable. The proper approach can make it easier to decrease the severity of symptoms, manage Hashimoto's thyroiditis more effectively, and improve the overall quality of life.
What many women don’t know is that they can manage estrogen dominance in a natural way, just by making certain lifestyle adjustments. First, it is important to see the doctor mainly because symptoms of Hashimoto’s disease and estrogen dominance are quite similar.
If you don’t have Hashimoto’s thyroiditis at the moment and are experiencing the above-mentioned symptoms, your doctor will inform you whether you have this autoimmune condition or estrogen dominance.
Those with thyroid autoimmunity and hypothyroidism who still experience symptoms from this post despite their treatment should consult their doctor who will presume that underlying problems such as high estrogen and low progesterone could be to blame.
So, what are the options for women with estrogen dominance? They include:
- Keep weight in a healthy range because being overweight or obese puts you at a greater risk of hormonal imbalances, including estrogen dominance, and it also contributes to thyroid problems
- Exercise regularly and increase physical activity levels as a sedentary lifestyle is a major threat to the balance of hormones in the body
- Avoid exposure to endocrine disruptors and estrogenic compounds due to the fact they could further aggravate balance between estrogen and progesterone. Estrogenic compounds mimic estrogen and boost their levels, thus making it difficult to manage estrogen dominance and Hashimoto’s thyroiditis. Try to avoid products with harsh ingredients, harsh makeup, BPA
- Lower consumption of soy as it contains phytoestrogens that only contribute to already high estrogen levels in the body
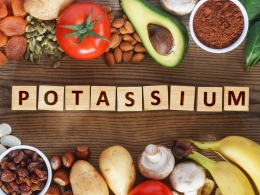
- Increase consumption of fruits and vegetables that deliver various nutrients to your body including antioxidants and anti-inflammatory benefits
- Consume enough fiber because it promotes healthy digestion. This is important because estrogen is excreted from the body via bowel movement. If estrogen remains in your stool, the body reabsorbs it. By eating more fiber, you can navigate around this problem
- Consult your doctor about progesterone cream that you can use to increase levels of progesterone and thereby balance estrogen concentration. Avoid using any hormone-based product without consulting your healthcare provider first
- Manage stress in order to prevent its negative impact on both thyroid hormone and estrogen levels. There are many ways one can manage stress, but you need to find something that makes you feel relaxed and keeps you calm. For each person, the stress relief method can be different. For example, exercise can be a wonderful stress management option just like reading, writing, yoga, meditation, hike, jogging, and you name it
Managing Hashimoto’s thyroiditis
Bearing in mind that Hashimoto's thyroiditis and estrogen dominance are similar, their treatment can involve almost the same measures.
Besides the adherence to doctor-recommended treatment (if prescribed), there are many lifestyle adjustments you can make to manage this condition. Weight management is one of those measures just like a well-balanced diet and regular exercise coupled with stress management.
Detox is equally important for both Hashimoto's and estrogen dominance. It's also important to avoid exposure to harsh ingredients and endocrine disruptors. Healing digestive tract is a significant aspect of Hashimoto's management, just like with estrogen dominance.
In other words, a healthy lifestyle is vital for proper management of both conditions.
Conclusion
Estrogen dominance occurs when there is too much estrogen in the body and little to no progesterone.
Millions of women have this condition and experience a wide range of symptoms whose intensity varies from mild to severe.
Estrogen dominance is strongly associated with Hashimoto’s thyroiditis, but more studies on this subject are necessary.
Unmanaged estrogen dominance can aggravate Hashimoto's disease, which is why it's important to address it properly.
Bearing in mind that two conditions have the same symptoms, you should consult your doctor who will order necessary tests to uncover the main cause of changes you experience.
References
[i] Patel S, Homaei A, Raju AB, Meher BR. (2018). Estrogen: The necessary evil for human health, and ways to tame it. Biomedicine and Pharmacotherapy, 102:403-411. Doi: 10.1016/j.biopha.2018.03.078. Retrieved from: https://www.ncbi.nlm.nih.gov/pubmed/29573619
[ii] Arduc A, Aycicek DB, Bilmez S, et al. (2015). High prevalence of Hashimoto's thyroiditis in patients with polycystic ovary syndrome: does the imbalance between estradiol and progesterone play a role? Endocrine Research, 40(4):204-10. Doi: 10.3109/07435800.2015.1015730. Retrieved from: https://www.ncbi.nlm.nih.gov/pubmed/25822940
[iii] Santin, A. P., & Furlanetto, T. W. (2011). Role of estrogen in thyroid function and growth regulation. Journal of thyroid research, 2011, 875125. doi:10.4061/2011/875125. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3113168/
[iv] Wang SH, Myc A, Koenig RJ, et al. (2000). 2-Methoxyestradiol, an endogenous estrogen metabolite, induces thyroid cell apoptosis. Molecular and Cellular Endocrinology, 165(1-2):163-72. Doi: 10.1016/s0303-7207(00)00249-5. Retrieved from: https://www.ncbi.nlm.nih.gov/pubmed/10940494


























































Leave a comment