Hypothyroidism and Low Testosterone
The thyroid hormone and the male reproductive system might be far apart from each other, but they are actually interrelated.
In fact, disturbances in thyroid function in men could have dire consequences on their sexual and reproductive functions.
Here we will explore more about the relationship between hypothyroidism and low testosterone levels, and how unprecedented changes in each can lead to disturbances in both thyroid and sexual functioning.
Thyroid Hormones and Its Effects on the Male Reproductive System
To understand the relationship between hypothyroidism and low testosterone levels, we first need to understand how the thyroid hormones affect the male reproductive system.
In a nutshell, there are a number of thyroid hormone receptors in the areas to be discussed below.
An increase or decrease of thyroid hormones flooding the said receptors can lead to the following changes:
Testicles
The testes – also known as testicles – are oval-shaped reproductive organs housed in a sac called the scrotum.
It serves as the storage house of sperm until maturity, but its most important responsibility is producing the hormone testosterone.
Thyroid hormones affect two types of cells in the testes. First is the Sertoli cell group, which sustains the development of germ cells. Its number is indicative of the testis’ daily production of sperm.
The hormone T3 affects the Sertoli cells through a number of activities. It suppresses the expression of immature Sertoli cell markers while it increases the level of cell cycle inhibitory proteins.
Additionally, the hormone T3 regulates the levels of gap junction proteins, thereby maintaining inter-Sertoli cell junctions.
Thyroid hormones also affect the development of Leydig cells, which are responsible for the production of testosterone under the control of the Luteinizing hormone.
In a study of hypothyroid rats, those exposed to propylthiouracil showed an increase in Leydig cell count.
However, this increase was due to the proliferation of immature Leydig cells, which have lower steroid production capacity and a smaller number of hCG binding sites. This brought the researchers into the conclusion that the hormone T3 is vital for the differentiation of mesenchymal cells into Leydig cells.
The steroidgenesis of Leydig cells is also affected by T3 concentration. Studies show that increased levels of thyroid hormones stimulate androgen production.
As a result, testosterone and progesterone levels are augmented in the presence of high amounts of T3.
Sperm
Sperm is the reproductive cell line produced in the testes. Its main function is to fuse with the egg cell in a process called fertilization – with the end result being the development of a fetus.
One of the parameters for sperm is sperm count, or the amount of sperm cells in a man’s ejaculate.
Such is affected by thyroid hormones, as another study of rats rendered hypothyroid by PTU treatment showed that the condition led to an increase in testis weight and enhanced efficiency of daily sperm production.
Experts attribute this to the increase in the rate of follicle stimulating and luteinizing hormones, and the number of Sertoli cells. Apoptosis of germ cells, on the other hand, is decreased.
Thyroid hormones are also known to affect sperm morphology, a predictor of success in egg cell fertilization. Abnormalities such as a deformed head can affect the sperm’s ability to fertilize a mature egg cell.
Defects in the tail, on the other hand, can affect its motility. Unfortunately, both the thyroid disorders can lead to a decrease in the number of morphologically normal sperm cells.
Thyroid dysfunctions are also known to affect sperm motility, or the sperm’s ability to move.
Those with afflicted the aforementioned conditions have been known to display slower progressive sperm motility.
Another aspect affected by thyroid hormones is fertility itself. In a study of rats, results showed that exposure to Methimazole led to lower levels of testosterone and estradiol in the interstitial fluid.
Reproductive Tract and Sex-Accessory Glands
In the epididymis, thyroid hormones can affect its structure and secretory activity.
Hypothyroidism has been known to decrease the secretion of carinitine, glycerophosphotylcholine, and sialic acid.
The contractile activity of the vas deferens is also affected by the thyroid hormones. Thyroidectomized rats demonstrate inhibited contractile activity, although this was reversed following treatment with T4 hormone.
Rats made hypothyroid with PTU, on the other hand, showcased a decrease in seminal vesicle and prostate gland weight.
Because of thyroid hormones’ effect on cell growth, metabolism, and differentiation, they are known to affect prostate cancer risk as well. In a surprising silver lining, a study by Mondul et al has shown that hypothyroid men have a lower prostate cancer risk compared to euthyroid males.
Hypothyroidism and Low Testosterone Levels
As it has been established, thyroid hormones regulate a number of male reproductive functions. As such, disturbances in thyroid hormone levels – such as in the case of hypothyroidism – can lead to a number of reproductive issues.
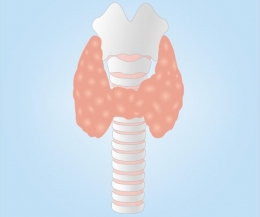
Hypothyroidism, or an underactive thyroid, occurs when the thyroid gland is unable to supply the body with its needed amount of hormones.
It occurs 10 times more in women (specifically older women) than in men. The prevalence in men is 1.3 to 4 per 1000 males.
A sufficient amount of thyroid hormones in the body is important, as they affect the rate of the body’s metabolism. With a low amount of thyroid hormones, your metabolism becomes slow and sluggish.
As such, hypothyroidism is hallmarked by the following signs and symptoms:
- Cold sensitivity
- Weight gain or inability to lose weight
- Slow heart rate
- Fatigue
- Dry hair and skin
- Depression
- Goiter
Apart from low thyroid hormone levels, the circulating testosterone levels also dip in patients with hypothyroidism.
One such research that proves this is the study of Donnelly and White. It featured ten men with primary hypothyroidism, an affliction that is known to disturb normal gonadal function. All showcased low free testosterone levels, however they increased following treatment with thyroxine.
This study posits that hypothyroidism affects gonadotropin secretion at the level of hypothalamus and pituitary gland, either through prolactin secretion or direct exertion.
Other causes that lead to a decrease of testosterone are the following:
- Low cholesterol uptake in the Leydig cells due to high cholesterol levels in serum
- Low conversion rate of progesterone to testosterone, as manifested through a low progesterone to testosterone ratio
- High conversation rate of estradiol to testosterone, as seen through an increased estradiol to testosterone ratio
- Hyperprolactinemia, where high prolactin levels lead to a slowed conversion of progesterone
- Low sex hormone-binding globulin levels
The high TSH and low thyroid hormone levels, as seen in hypothyroid men, are also known to inhibit testosterone steroidgenesis.
Unfortunately, these low testosterone levels can contribute to some signs and symptoms of hypothyroidism in men, which include hypoactive sexual desire, ejaculatory disorders and erectile dysfunction.
The Effects of Low Testosterone Levels
Testosterone is more than just a sexual hormone, it is important for cognition and body development as well.
Testosterone is converted from cholesterol in the Leydig cells via a sophisticated feedback system that starts with the hypothalamus.
Low testosterone levels usually happen as men age, although there are a variety of factors that can cause this as well. Apart from hypothyroidism, obesity, diabetes mellitus, chronic illness, cancer, depression, and use of certain medications can lead to a decrease in testosterone levels as well.
The normal level of testosterone in a man’s body is somewhere from 300 to 800 ng/dl. If it falls below 300 ng/dl, the following signs of androgen deficiency can develop:
- Incomplete or delayed development of sexual characteristics
- Decreased erections (spontaneous)
- Gynecomastia
- Slower growth of pubic or axillary hair
- Testes measuring less than 5 ml
- History of infertility
- Oligospermia (low sperm count) or aspermia (lack of sperm in semen)
- History of fracture or low bone mineral density
- Anemia
- Weight gain
- Low libido
- Breast discomfort
- Tiredness and fatigue
- Depressed mood
Because of the many afflictions that can lead to low testosterone levels, certain diagnostic exams need to be done to determine if it is caused by hypothyroidism.
The study of Crawford and Kennedy recommend the measurement of serum free thyroxine (T4) or free thyroxine index (FTI) in concomitance with a TSH test.
While the effects of low testosterone levels can be alarming to any man, the fact of the matter is they can be reversed with thyroid hormone supplementation – granted that the cause of the low levels is hypothyroidism.
Many studies have proven that levothyroxine therapy is effective in boosting testosterone levels, apart from minimizing, if not eliminating the associated unpleasant symptoms.
Low Testosterone Levels Affect Women as Well
Testosterone is widely associated with men, but this hormone is important for the female body as well.
It is responsible for producing new cells, as well as influencing the hormones that affect reproduction. Similar to its use in men, testosterone can affect a woman’s libido.
Testosterone is produced in the ovaries alongside estrogen, with minute quantities released in the circulation as needed.
Similar to men, a woman’s testosterone levels decreases with aging. Levels of 25 ng/dl and below are considered low for women aged 50 and below, while levels of 20 ng/dl and below are alarming for women aged 50 years old and above.
Testosterone levels in women can dip due to early menopause, estrogen therapy, surgical removal of the ovaries, adrenal insufficiency, or hypopituitarism. When such levels drop, the following signs and symptoms can develop:
- Low sexual desire and satisfaction
- Lethargy
- Depression
- Muscle weakness
Similar to men, low testosterone levels in women caused by hypothyroidism can be easily resolved with hormone supplementation.
Hyperthyroidism and the Testosterone Connection
Just like hypothyroidism, hyperthyroidism, a disorder marked by an increased production of thyroxine, affect normal male sexual reproductive processes as well.
Hyperthyroidism, or an overactive thyroid, occurs when the body produces excessive amounts of the thyroid hormone thyroxine. With more thyroid hormones in the body, your metabolic activity can be launched into overdrive.
With a higher metabolic rate, hyperthyroid patients often experience sudden weight loss, rapid and irregular heartrate, irritability, nervousness, and profuse sweating, to name a few.
As with thyroid hormone levels, hyperthyroidism brings about an increase in testosterone and estradiol levels as well. Because of the increase in circulation brought about by the metabolic effects of hyperthyroidism, more testosterone is delivered to the peripheral tissues, which is then aromatized into estradiol.
Another hormone that is markedly increased in hyperthyroid men is sex hormone-binding globulin, which leads to a decrease in testosterone clearance rate. This is considered as one of the factors behind the increased testosterone levels associated with hyperthyroidism.
Expectedly, the high testosterone levels lead to some hyperthyroidism symptoms, such as gynecomastia or the enlargement of breast tissue in men.
Thyroid dysfunction affects many parts of the body. With hypothyroidism altering testosterone levels to subpar levels – your sexual health and fertility are at risk. With that being said, if you experience any symptoms that might be associated to a thyroid disorder – have it checked by your physician right away.
References
Ariyaratne HB, Mills N, Mason IJ, Mendis-Handagama SM. Effects of thyroid hormone on Leydig cell regeneration in the adult rat following ethane dimethane sulphonate treatment. Biol Reprod. 2000;63:1115–23.
Crawford, M., & Kennedy, L. (2016). Testosterone replacement therapy: role of pituitary and thyroid in diagnosis and treatment. Translational Andrology and Urology, 5(6), 850–858. http://doi.org/10.21037/tau.2016.09.01
Donnelly, P., & White, C. (2000). Testicular dysfunction in men with primary hypothyroidism; reversal of hypogonadotrophic hypogonadism with replacement thyroxine. Clinical Endocrinology,52(2), 197-201. doi:10.1046/j.1365-2265.2000.00918.x
Kumar, A., Shekhar, S., & Dhole, B. (2014). Thyroid and male reproduction. Indian Journal of Endocrinology and Metabolism, 18(1), 23–31. http://doi.org/10.4103/2230-8210.126523
Kumar, P., Kumar, N., Thakur, D. S., & Patidar, A. (2010). Male hypogonadism: Symptoms and treatment. Journal of Advanced Pharmaceutical Technology & Research, 1(3), 297–301. http://doi.org/10.4103/0110-5558.72420
Mondul AM, Weinstein SJ, Bosworth T, Remaley AT, Virtamo J, Albanes D. Circulating thyroxine, thyroid stimulating hormone, and hypothyroid status and the risk of prostate cancer. PLOS One. 2012;7:1–7.
Vanderpump, M. P. (2011). The epidemiology of thyroid disease. British Medical Bulletin,99(1), 39-51. doi:https://doi.org/10.1093/bmb/ldr030

























































Leave a comment