Hypothyroidism and Hypoglycemia Relationship
Hypothyroidism and hypoglycemia have much in common, although they are very different conditions. Both are metabolic disorders with one affecting the thyroid gland and the other one affecting glucose metabolism.
Though seemingly unrelated, hypothyroidism brings about mechanisms that result in hypoglycemia, as problems in glucose maintenance (such as diabetes) can occur alongside hypothyroidism.
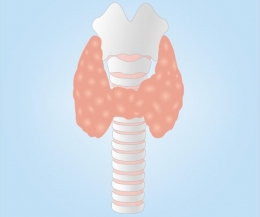
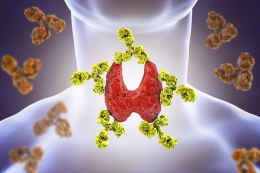
What is Hypothyroidism?
First, we need to delve more into the world of hypothyroidism.
This condition is hallmarked by the thyroid gland’s inability to produce the proper amount of thyroid hormones that the body needs. As a result, body functions slow down.
Hypothyroidism, the most common thyroid condition, occurs frequently in women and in people aged 60 years old and above.
According to the National Institutes of Health, approximately 4.6% of the American population aged 12 years old and older suffer from this disorder.
Hypothyroidism can be caused by any of the following:
- Hashimoto’s Thyroiditis. This is the most common cause of hypothyroidism in the United States. This autoimmune condition brings about low thyroid hormone production.
- Characterized by an inflammation of the thyroid gland, this leads to the leakage of thyroid hormones in the circulation. Initially it leads to hyperthyroidism, which lasts for one to two months, before progressing to hypothyroidism.
- Congenital Hypothyroidism. This condition is found in babies who have underdeveloped or improperly-functioning thyroid glands. If left undetected, it can lead to growth failure and mental retardation.
Below are risk factors that can lead to the development of hypothyroidism:
- Family history of thyroid disorders
- Goiter
- Pregnancy or childbirth within the last six months
- Diagnosis of autoimmune diseases such as type 1 diabetes, pernicious anemia, rheumatoid arthritis, lupus, or Sjogren’s syndrome
- Diagnosis of Turner’s syndrome, a genetic condition found in women
The following conditions can result in hypothyroidism as well:
- Thyroid Surgery. Removal of part or the entire thyroid gland is done to treat hyperthyroidism, goiter, nodules, or cancer.
- Radiation Therapy. This common treatment for hyperthyroidism works by gradually destroying the thyroid gland, as a result most who undergo this procedure develop hypothyroidism. Those who receive radiation therapy targeted for head and neck cancers, lymphomas, and Hodgkin’s disease can develop hypothyroidism as well.
- Hypothyroidism can occur in early pregnancy and during the postpartum period. For those with preexisting thyroid problems, the state of pregnancy will necessitate an increase in the intake of thyroid medications. In 10% of women, postpartum thyroiditis can occur within the first year of delivery. This autoimmune condition is oftentimes mistaken as exhaustion and mood swings that follow after childbirth. If left undetected and untreated, this condition can lead to permanent hypothyroidism.
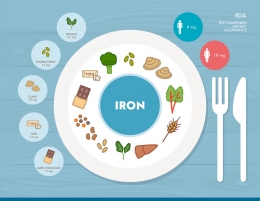
- Low intake of dietary iodine
- Pituitary gland abnormalities or disorders
- Intake of certain medications such as Interferon Alpha, Interleukin-2, Lithium, and Amiodarone
What is Hypoglycemia?
Commonly known as low blood sugar or low blood glucose, this condition is characterized by a blood sugar level lower than 70 milligrams/deciliter.
Symptoms vary according to severity. Mild to moderate hypoglycemia is considered when the following take place:
- Headaches
- Hunger
- Sweating
- Blurring of vision
- Pallor
- Uncoordinated body movements
- Weakness
- Fast or irregular heartbeats
- Dizziness or lightheadedness
- Confusion or disorientation
- Irritability or nervousness
- Argumentative or combative behavior
- Change in behavior or personality
- Shakiness, jitters
- Tiredness or sleepiness
Severe hypoglycemia, on the other hand, occurs commonly in type 1 diabetics. It often comes with the following symptoms:
- Inability to drink or eat
- Loss of consciousness
- Convulsions or seizures
Hypoglycemia often occurs in diabetic individuals due to the intake of insulin and medications such as meglitinides and sulfonlyureas. Other causes for hypoglycemia include:
- Lack of carbohydrates in the diet. Carbohydrates are transformed to glucose by the digestive system. If there are not enough carbs to match the intake of diabetes medication, hypoglycemia can develop.
- Delayed or skipped meals. This leads to hypoglycemia as there is less glucose for the body to work with whenever you are asleep or if you have forgotten to eat on time.
- Increased physical activity. Strenuous exercise or activity can lead to hypoglycemia, as more energy is used compared to the glucose intake. Hypoglycemia following increased physical activity can occur even after 1 day after the workout.
- Alcohol drinking without food intake. Alcohol makes blood glucose regulation difficult for the body. Additionally, its effects can mask the symptoms of hypoglycemia.
- Sickness. An ailment that impairs food intake can lead to hypoglycemia.
Hypoglycemia can occur in non-diabetics as well.
Compared to its diabetic counterparts, non-diabetic hypoglycemia is characterized by a blood sugar level of less than 55 mg/dl. It comes in two forms, namely:
- Reactive Hypoglycemia
- May be brought about by pre-diabetes, where there is a problem making sufficient amounts of insulin.
- May be caused by a stomach operation wherein food is digested immediately and propelled quickly to the small intestine.
- Can be caused by enzyme deficiencies that make it hard to break down food, as such glucose content found in food is not readily utilized.
- Fasting Hypoglycemia
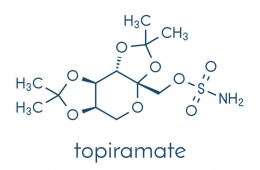
- Can result from the side effect of medications such as pentamidine, quinine, salicylates, and sulfa drugs.
- Can be a result of alcohol drinking, especially binge drinking.
- May result from serious illnesses affecting the heart, liver, or kidneys.
- May result from low levels of certain hormones such as epinephrine, cortisol, glucagon, and growth hormone.
- May result from pancreatic tumors or tumors that secrete IGF II-like hormones.
Hypothyroidism and Hypoglycemia
According to an article by Dr. Patricia Wu, diabetic patients have a higher prevalence of thyroid dysfunction, in comparison to the ‘normal’ population. In fact, it occurs in as much as 30% of women with type 1 diabetes, mainly because of the fact that thyroid dysfunction is more common in females.
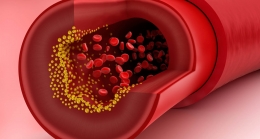
Because of the thyroid gland’s role in regulating metabolism, problems in thyroid function can have an adverse effect on glucose regulation and diabetes control. If thyroid disorders are left untreated, diabetes symptoms can worsen and untoward complications might develop.
Hypothyroidism, which is one of the most common endocrine disorders in the planet, often coexists with diabetes types 1 and 2. In fact, a study by Palma et al showed that approximately of 14.7% of participating diabetic patients in the research exhibited diabetes dysfunction.
While hyperglycemia might be the first thing to come in mind when diabetes is mentioned, the fact of the matter is hypoglycemia is often seen in such patients. This can be traced to the fact that hypothyroidism is a precipitating factor for hypoglycemia. According to Kalra et al, the numerous biochemical and nervous system abnormalities linked with hypothyroidism usually lead to hypoglycemia.
Hypoglycemia is worsened in hypothyroid patients due to the following reasons:
- Since hypothyroidism acts on the hypothalamus and the pituitary gland, there is a reduction in basal and growth hormone levels. Because of this response, recovery from hypoglycemia takes a longer time in hypothyroid patients.
- Hypothyroid patients also suffer from relative adrenal insufficiency. Consequently, there is a problem with the hypothalamo-pituitary-adrenal response to hypoglycemia, so recovery from the said condition is slower.
- Gluconeogenesis, or the creation of glucose from protein, fat, or lactate is impaired, especially in the skeletal muscle and adipose tissue. Glycogenolysis, on the other hand, which is the breakdown of glycogen to glucose, is slowed down in hypothyroid patients. Both discrepancies lead to blood sugar levels lower than normal.
- In hypothyroidism, secretion of glucagon, a hormone produced by the Alpha cells of the pancreas secretion, is reduced. Its effect on the hepatocytes are lessened as well. As a result, the breakdown of fat and glycogen into usable glucose is delayed.
- Insulin clearance is often slowed down in hypothyroidism. The more insulin there is in the blood stream, the lower the blood glucose levels will be.
- Hypothyroidism also brings about changes in the gastrointestinal system that lead to hypoglycemia. Examples include slowed gastric emptying, decreased glucose absorption in the intestines, and impaired portal venous flow.
- Thyroid hormones are said to exert agonistic effects on insulin in the peripheral tissues. As a result, blood sugar levels are kept at a low level.
Due to the relationship between hypothyroidism and hypoglycemia, people with low glucose symptoms without remarkable cause should be checked for thyroid function.
This was reflected in case study done by Yadav et al, where a 32-year-old female demonstrated weakness, fatigue, palpitation, and sweating, despite not having a history of chronic illness.
Numerous diagnostic exams were done, but no apparent cause of hypoglycemia was found. Her serum insulin and C-peptide levels came out negative, thereby discounting the possibility of insulinoma or islet cell hypertrophy.
Autoimmune causes of hypoglycemia were ruled out as well.
Baffled with her condition, the doctors diagnosed her as a case of Primary Adrenal Insufficiency. But despite continuous treatment with hydrocortisone, her hypoglycemic episodes continued.
As such, she underwent MRI, tests for follicle-stimulating and luteinizing hormone, as well as a thyroid profile.
All came back negative except for an elevation in TSH and a reduction in T3 and T4 levels. With these results cementing the diagnosis of hypothyroidism, she was placed on a regimen of 50 mcg of Thyroxine two times a day.
Six weeks after treatment, unsurprisingly, no hypoglycemic episodes took place anymore. Expectedly, her thyroid profile improved as well.
Implications for Treatment
For diabetics, in the event that there is an increase in the severity or frequency of hypoglycemia, which cannot be blamed on diet, physical activity, or intake of antidiabetic drugs, the possibility of hypothyroidism should be considered. Similarly, hyperthyroidism should be considered in diabetic individuals with worsening hyperglycemia without any probable cause.
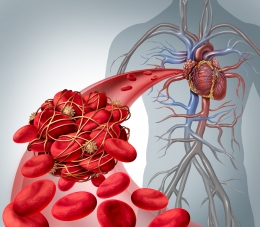
More than just low blood sugar, hypoglycemia in hypothyroid patients on diabetes treatment can signify possible neuroglycopenia. This defect can develop due to problems in the release of regulatory hormones in hypothyroid individuals.
Because of these events, much care should be taken into consideration when prescribing hypothyroid patients with diabetes treatment.
Due to the effects of hypothyroidism on glucose regulation in the body, lower doses of insulin and sulfonylureas (insulin secretagogues) should be prescribed to hypothyroid patients. If possible, safer insulin analogues should be given as they carry lower incidences of hypoglycemia compared to other diabetes medications.
More importantly, thyroid status should be evaluated regularly in the course of diabetes treatment as dose adjustments might be needed every so often. After all, Metformin exerts a thyroprotective effect and can lead to a decrease in TSH levels.
As such, individuals with decreasing TSH levels or improving thyroid status might necessitate an increase in dose, while those with declining thyroid status might need a decrease in antidiabetic medication dosage.
Recognizing and treating hypothyroidism in its early stages are particularly important in patients with type 2 diabetes.
After all, hypothyroidism brings about an increase in triglyceride and low-density lipoprotein, and can worsen the lipid problems associated with type 2 diabetes. By treating hypothyroidism early at its tracks, the compounding cardiovascular risks can be lessened tremendously.
References:
Hypothyroidism: The Thyroid and You | NIH MedlinePlus the Magazine. (n.d.). Retrieved June 6, 2018, from https://medlineplus.gov/magazine/issues/spring12/articles/spring12pg22-23.html
Kalra, S., Unnikrishnan, A. G., & Sahay, R. (2014). The hypoglycemic side of hypothyroidism. Indian Journal of Endocrinology and Metabolism, 18(1), 1–3. http://doi.org/10.4103/2230-8210.126517
Low Blood Glucose (Hypoglycemia). (2016, August 01). Retrieved June 10, 2018, from https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/low-blood-glucose-hypoglycemia
Nondiabetic Hypoglycemia. (n.d.). Retrieved June 10, 2018, from https://www.hormone.org/diseases-and-conditions/diabetes/non-diabetic-hypoglycemia
Palma, C. C. S. S. V., Pavesi, M., Nogueira, V. G., Clemente, E. L. S., Vasconcellos, M. de F. B. M. P., Pereira, L. C., … Gomes, M. B. (2013). Prevalence of thyroid dysfunction in patients with diabetes mellitus. Diabetology & Metabolic Syndrome, 5, 58. http://doi.org/10.1186/1758-5996-5-58
Wu, P. (n.d.). Thyroid Disease and Diabetes. Retrieved from http://journal.diabetes.org/clinicaldiabetes/v18n12000/pg38.htm
Yadav, T., Bhutani, J., Upadhyay, M., & Raghunandan, S. (2017). Recurrent hypoglycemia: An unusual finding of hypothyroidism. Thyroid Research and Practice,14(3), 127-129. Retrieved June 11, 2018, from http://www.thetrp.net/article.asp?issn=0973-0354;year=2017;volume=14;issue=3;spage=127;epage=129;aulast=Yadav


























































Leave a comment